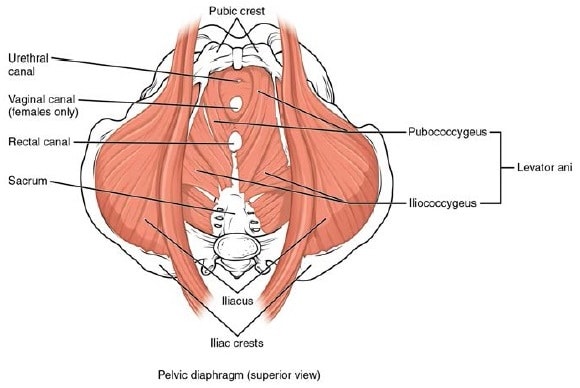
The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
It is important in providing support for pelvic viscera (organs), e.g. the bladder, intestines, the uterus (in females), and in maintenance of continence as part of the urinary and anal sphincters. It facilitates birth by resisting the descent of the presenting part, causing the fetus to rotate forwards to navigate through the pelvic girdle. It helps maintain optimal intra-abdominal pressure.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling. Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border). The perineum has the pelvic floor as its superior border.
Some sources do not consider “pelvic floor” and “pelvic diaphragm” to be identical, with the “diaphragm” consisting of only the levator ani and coccygeus, while the “floor” also includes the perineal membrane and deep perineal pouch. In practice, the two terms are often used interchangeably.
Posteriorly, the pelvic floor extends into the anal triangle.
The pelvic floor has two hiatuses (gaps): Anteriorly urogenital hiatus through which urethra and vagina pass through and posteriorly rectal hiatus through which anal canal passes.
In pregnancy
The pelvic floor supports the bladder, bowel, and uterus, and gives the mother control over when she empties her bladder and bowel.
Having a weak pelvic floor makes it harder to squeeze the muscles and sphincters at the bottom of the bladder to prevent urine from escaping. Since pregnancy and childbirth puts a great deal of stress on the muscles of the pelvic floor many women experience stress incontinence after childbirth. This means they accidentally release a small amount of urine when they cough, laugh, sneeze or exercise.
Doing pelvic floor exercises can help to treat bladder weakness or prolapse symptoms, and will help to prevent problems later on.
OpenStax, Anatomy & Physiology. OpenStax. 25 April 2013.
Pelvic floor. (2016, September 20). In Wikipedia, The Free Encyclopedia. Retrieved 22:17, September 20, 2016, from https://en.wikipedia.org/w/index.php?title=Pelvic_floor&oldid=740410864
