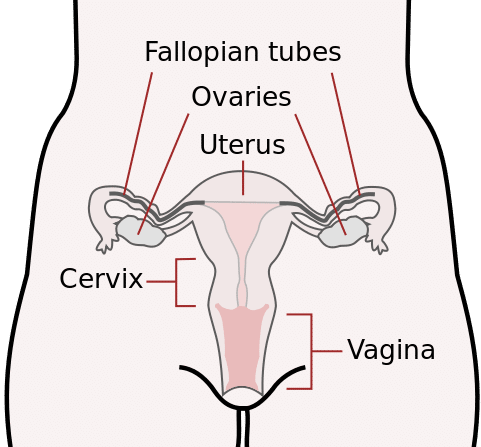
The cervix or cervix uteri (Latin: neck of the uterus) is the lower part of the uterus in the human female reproductive system. In a non-pregnant woman, the cervix is usually 2 to 3 cm long (~1 inch) and roughly cylindrical in shape. The narrow, central cervical canal runs along its entire length, connecting the uterine cavity and the lumen of the vagina. The opening into the uterus is called the internal os, and the opening into the vagina is called the external os. The lower part of the cervix, known as the vaginal portion of the cervix (or ectocervix), bulges into the top of the vagina. The cervix has been documented anatomically since at least the time of Hippocrates, over 2,000 years ago.
The cervical canal is a passage through which sperm must travel to fertilize an egg cell after sexual intercourse. Several methods of contraception, including cervical caps and cervical diaphragms aim to block or prevent the passage of sperm through the cervical canal. Cervical mucus is used in several methods of fertility awareness, such as the Creighton model and Billings method, due to its changes in consistency throughout the menstrual period. During vaginal childbirth, the cervix must flatten and dilate to allow the fetus to progress along the birth canal. Midwives and doctors use the extent of the dilation of the cervix to assist decision-making during childbirth.
The cervix plays a major role in childbirth. As the fetus descends within the uterus in preparation for birth, the presenting part, usually the head, rests on and is supported by the cervix. As labor progresses, the cervix becomes softer and shorter, begins to dilate, and rotates to face the anterior. The support the cervix provides to the fetal head starts to give way when the uterus begins its contractions. During childbirth, the cervix must dilate to a diameter of more than 10 cm (3.9 in) to accommodate the head of the fetus as it descends from the uterus to the vagina. In becoming wider, the cervix also becomes shorter, a phenomenon known as effacement.
Along with other factors, midwives and doctors use the extent of cervical dilation to assist decision making during childbirth. Generally, the active first stage of labor, when the uterine contractions become strong and regular, begins when the cervical dilation is more than 3–5 cm (1.2–2.0 in). The second phase of labor begins when the cervix has dilated to 10 cm (4 in), which is regarded as its fullest dilation, and is when active pushing and contractions push the baby along the birth canal leading to the birth of the baby. The number of past vaginal deliveries is a strong factor in influencing how rapidly the cervix is able to dilate in labor. The time taken for the cervix to dilate and efface is one factor used in reporting systems such as the Bishop score, used to recommend whether interventions such as a forceps delivery, induction, or Caesarean section should be used in childbirth.
Cervical incompetence is a condition in which shortening of the cervix due to dilation and thinning occurs, before term pregnancy. Short cervical length is the strongest predictor of preterm birth.
CDC, Mysid Female Cervix (Public Domain)
